Pathogenesis
The pathogenic E. coli within each pathotype may be further classified as virotypes, based on the virulence genes that they possess. A virotype is a particular combination of virulence genes. Important virulence factors encoded by these genes include fimbrial adhesins, enterotoxins, cytotoxins, capsule, and lipopolysaccharide, or LPS. Pathogenic E. coli may also be differentiated by serotypinc, based on antigenic differences in the O antigen of the LPS, in the flagellar or H antigens, and the fimbrial or F antigens.
The following diagrams show how pathogenic E. coli of each pathotype cause disease. Follow the appropriate links to learn which virulence factors are involved in each step of the disease process, and what are the important O serotypes and virotypes.
ETEC
Pathogenic bacteria contaminating the environment are ingested by susceptible animals and enter the intestinal tract (1). These bacteria possess fimbrial adhesins which mediate adherence to specific receptors on the intestinal epithelial cells (2). Resulting bacterial colonization is found mostly on the jejunal and or ileal mucosa. The adherent bacteria produce enterotoxins which stimulate water and electrolyte loss into the intestinal lumen (3), leading to dehydration and possibly death, and a decreased weight gain in surviving animals (4).
>> Click here to see fimbriated bacteria adhere to intestinal border
STEC Edema disease
Pathogenic bacteria contaminating the environment are ingested by susceptible animals and enter the intestinal tract (1). These bacteria possess fimbrial adhesins which mediate adherence to specific receptors on the intestinal epithelial cells (2). Resulting bacterial colonization is found mostly on the jejunal and or ileal mucosa. The adherent bacteria produce a toxin which is transported across the epithelial cells to the circulation (3). This toxin acts on the endothelial cells of blood vessels, resulting in edema in different tissues, leading to the manifestation of such symptoms as ataxia and death (4).
>> Click here to see fimbriated bacteria adhere to intestinal border
EPEC
Pathogenic bacteria contaminating the environment are ingested by susceptible animals and enter the intestinal tract (1). Focal to extensive bacterial colonization of small and large intestine is observed (2). Bacteria produce their own specific receptor which is injected into the host epithelial cell via a syringe-like bacterial apparatus. A bacterial adhesin then mediates a very intimate attachment of the bacteria to the cell receptors and bacterial signals stimulate effacement of the microvilli, or brush border, and reorganization of the cell cytoskeleton (3). The adherent bacteria also stimulate epithelial cell degeneration, and infiltration of PMN's in lamina propria. These cell changes may lead to the appearance of diarrhea (4).
>> Click here to see a transmission electron micrograph (TEM) of stages of bacterial attachment and effacement of weaning pig
>> Click here to see a transmission electron micrograph (TEM) of E. coli intimately attached to ileal epithelial cells of pigs with effacement of the microvilli
ExPEC
Potentially pathogenic bacteria contaminating the environment are ingested by susceptible animals and enter the intestinal tract or enter via the respiratory tract (chickens) (1). These bacteria are considered to be opportunistic pathogens, as they remain as part of the normal microflora and colonize intestinal, respiratory or other mucosal surfaces, possibly due to fimbrial adhesins (2).
When the animal is weakened, such as following a viral infection, due to ingestion of mycotoxins, or when a newborn has not received enough colostrum, bacteria pass more readily through the mucosa to the circulation (3). These internalized bacteria can resist the lethal effects of complement and phagocytes (4) and persist and multiply in the system (5 also in part due to the production
of aerobactin. The production of toxins by the bacteria may contribute to tissue damage (6). Release of endotoxins by dead bacteria, may trigger cytokine responses leading to shock and death of the animal (7). In localized infections, there may be bacterial interaction with extracellular matrices, leading to pneumonia, serositis, mastitis, urinary tract infection, etc. (8).
>> Click here to see a transmission electron micrograph (TEM) of association of ExPEC with mucus layer in intestine in the pig
>> Click here to see in situ visualization of bacterial translocation of ExPEC of intestinal submucosa in the pig
>> Click here to see in situ visualization of spread of ExPEC bacteria and localization in extraintestinal sites
>> Click here to see a light micrograph of ExPEC bacterial colonization of the trachea in a chicken
>> Click here to see a transmission electron micrograph (TEM) of ExPEC bacterial colonization and translocation through the epithelial layer of the air sacs in a chicken
>> Click here to see a light micrograph of ExPEC bacterial contact with complement and other extracellular components in the connective tissue of a chicken
>> Click here to see a transmission electron micrograph (TEM) of ExPEC bacterial contact with collagen fibres in the interstitium of the air sacs of a chicken
>> Click here to see a transmission electron micrograph (TEM) of intracellular ExPEC bacteria in phagocytes in the air sacs of a chicken
>> Click here to see a transmission electron micrograph (TEM) of extracellular ExPEC bacteria in contact with phagocytes in the lung of a chicken
>> Click here to see an association and viability of ExPEC strains and various mutants in contact with heterophils and macrophages in primary culture
STEC Ruminants and contamination cycle
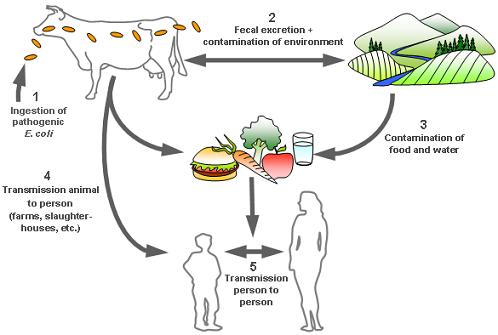
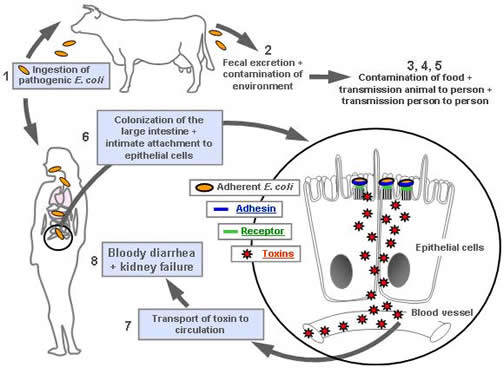
Potentially pathogenic bacteria are ingested by cattle and other ruminants (1) and colonize the intestinal tract, but do not cause any disease in these animals. The bacteria are excreted in the feces and contaminate the environment, including the drinking and swimming water of the human population (2). There may also be contamination of foods such as fruits, vegetables, sprouts, lettuce, and raw milk and juice (3). There may be contamination of the carcass at slaughter, and bacteria will be mixed into ground beef.
Persons in direct contact with animals, who are working on farms or in slaughter-houses, may also be contaminated by the bacteria (4).
There may also be spread of bacteria from person to person (5). In humans, these bacteria colonize mostly the large intestine and cause similar attaching and effacing lesions to those described for AEEC (6). Bacteria produce their own specific receptor which is injected into the host epithelial cell via a syringe-like bacterial apparatus. A bacterial adhesin then mediates a very intimate attachment of the bacteria to the cell receptors and bacterial signals stimulate effacement of the microvilli, or brush border, and reorganization of the cell cytoskeleton. The adherent bacteria produce a toxin which is transported across the epithelial cells to the circulation (7). This toxin acts on the endothelial cells of blood vessels, resulting in nonbloody to bloody diarrhea and abdominal cramps (8). There may be a complication of hemolytic uremic syndrome which may lead to acute kidney failure, especially in children.
 Top of page
Top of page